In July 2025, the UK government unveiled its ambitious NHS 10-Year Plan, titled Fit for the Future, aiming to transform the National Health Service into a more resilient, efficient, and patient-centred system.
With public satisfaction at historic lows and mounting pressure on services, this plan represents a pivotal moment in the evolution of British healthcare.
The plan sets out a roadmap to shift care into communities, embrace digital tools, and focus on prevention.
For lawyers specialising in health law and healthcare professionals leading compliance, risk management and operations, the plan introduces new contractual considerations, regulatory requirements, and governance challenges. Grasping these changes will be essential for negotiating service agreements, safeguarding patient rights, and maintaining resilience in a rapidly evolving health landscape.
The plan was shaped through Change NHS, the largest public engagement initiative in NHS history. Over 250,000 contributions from patients, staff, and stakeholders helped inform the strategy.
At the heart of the plan are three transformative shifts:
- Hospital to community: decentralise care by investing in neighbourhood health centres and expanding GP access. This shift aims to reduce hospital admissions and bring care closer to where people live.
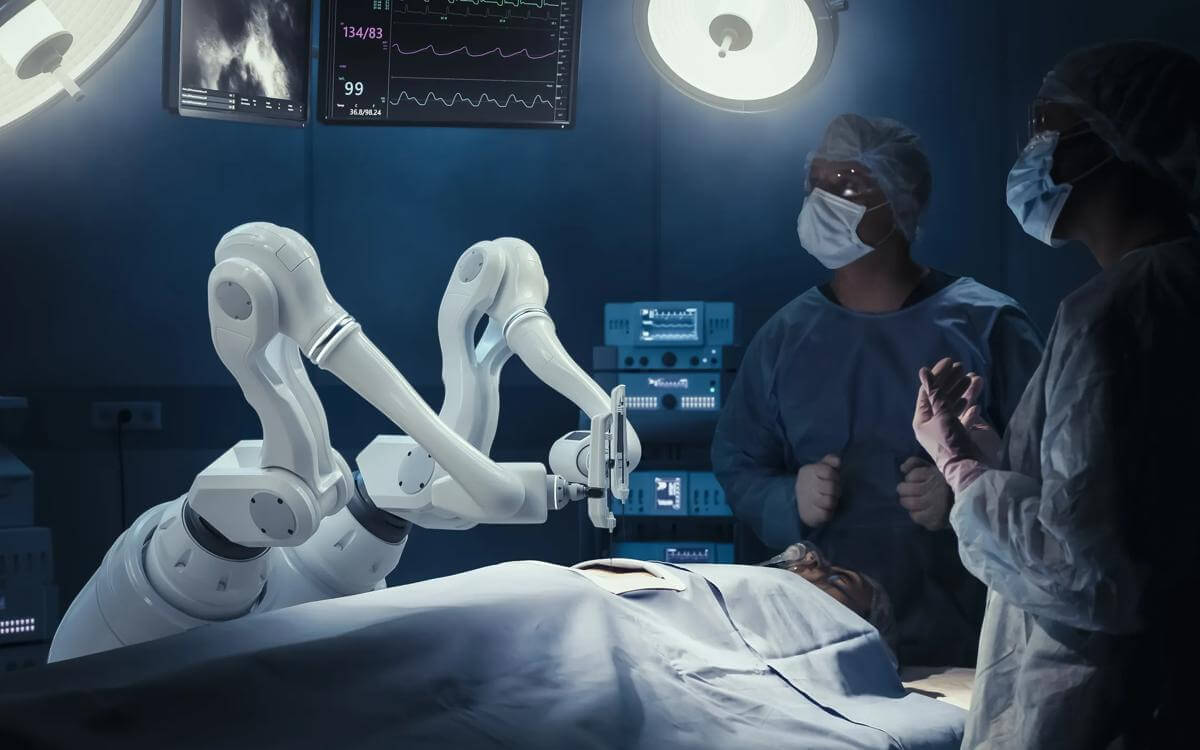
- Analogue to digital: A “digital-first” approach will modernise patient interactions. Upgrades to the NHS App will allow users to book tests, manage care, and access consultations online, improving convenience and reducing administrative burdens.
- Sickness to prevention: By focusing on preventative care, the NHS hopes to reduce long-term illness and improve public health outcomes. This includes bolstering community rehabilitation services and promoting healthier lifestyles.
At Browne Jacobson, we represent both the public and private sectors and appreciate the challenges and opportunities both will face in helping to deliver on the plan.
Significant hurdles
Despite its bold vision, the plan faces significant hurdles. Critics argue that previous reform efforts have struggled with implementation. A number of the issues faced are summarised below.
Strategic objectives and commissioning reforms
The plan commits to moving care upstream - expanding primary care networks and integrated care systems - and linking payment to health outcomes rather than activity volume. Key commissioning changes include:
- Shared-risk contracts across NHS trusts, local authorities, and third-sector partners.
- Outcome-based schedules prioritising prevention metrics.
- Enhanced data-sharing obligations to support population health management.
Legal teams must scrutinise liability and indemnity provisions, confirm alignment with the NHS Standard Contract and national tariff rules. They will also need to advise on dispute-resolution mechanisms as providers enter blended-funding arrangements.
Workforce agreements and professional practice
A major component of the plan is the creation of a new workforce model. The government aims to align staff roles with future needs, addressing recruitment and retention challenges - especially in primary care nursing. The plan also calls for investment in flexible, modular healthcare facilities to expand capacity quickly and cost-effectively.
Addressing workforce shortages, the plan introduces multi-disciplinary roles, flexible contracts, and expanded scopes of practice under GMC and NMC oversight. Healthcare employers should expect:
- Revised employment terms accommodating digital-first consultations.
- Additional Roles Reimbursement Scheme extensions for allied health professionals.
- New apprenticeship pathways with integrated supervision requirements.
Lawyers advising on these contracts will need to balance evolving professional standards, employment law compliance, and indemnity coverage to mitigate risks of service interruptions or negligence claims.
Digital transformation and data governance
A “digital-first” ethos underpins the plan’s ambition to streamline referrals and remote monitoring. From a legal standpoint, critical considerations are:
- GDPR compliance for telehealth and patient-access platforms.
- Intellectual property rights for jointly developed AI tools and diagnostics.
- Cybersecurity obligations under NIS Regulations and NHS Digital standards.
Drafting robust data-sharing agreements, incident-response protocols, and clear consent frameworks will be vital to protect patient confidentiality and organisational reputation.
Funding structures, procurement, and financial liability
Significant capital investment is earmarked for community diagnostics hubs and modular facilities. Procurement and legal professionals must prepare for:
- Tender evaluations incorporating social-value and sustainability scoring
- Public–private partnership agreements with milestone-based funding releases
- Risk-sharing clauses addressing cost overruns and service quality shortfalls
Precise drafting of payment triggers, liability caps, and arbitration pathways will help organisations manage financial exposure and ensure continuity of care.
Risk management and regulatory compliance
New key performance indicators and national reporting duties demand enhanced governance. Organisations should:
- Update internal audit programmes to monitor integrated care outcomes.
- Revise clinical governance policies for community services.
- Train staff on changes under the Health and Social Care Act and related regulations.
Legal teams will support preparedness for regulatory inspections, enforcement actions, and patient-safety investigations, ensuring that policy ambitions translate into compliant practice.
The NHS 10-Year Plan offers a compelling roadmap for reform, rooted in innovation, prevention, and community care. If executed effectively, it could redefine healthcare delivery in England and restore public trust in the NHS. But success will depend on sustained investment, clear implementation strategies, and a continued commitment to listening to those who rely on and work within the system.
For lawyers and healthcare professionals, the NHS 10-Year Plan offers both opportunities and obligations.
By embedding rigorous contractual safeguards, strengthening data-governance frameworks, and reinforcing compliance systems, stakeholders can help deliver a more sustainable, patient-centred NHS.
Proactive, cross-disciplinary collaboration will be the key to transforming strategic goals into operational success, and at Browne Jacobson, our health and life sciences lawyers aspire for just that, for the next 10 years and beyond.