Technology-enabled care (“TEC”) – which includes remote monitoring, telecare, smart-home sensors and care-focused apps – has moved from niche pilot projects into mainstream health and social care across the UK.
Over the past 18 months, regulators, government and service providers have tightened technical expectations and legal guardrails, creating both new opportunities for growth and fresh compliance issues for suppliers and regulators.
MHRA's evolving regulatory framework
The Medicines and Healthcare products Regulatory Agency (“MHRA”) and the government have signalled a clearer, more prescriptive approach to software, AI and connected devices that perform clinical functions.
The MHRA’s evolving “future regulation” roadmap and its Software & AI as a Medical Device programme map out staged reforms – including revised post-market surveillance rules and dedicated guidance on cybersecurity for Software as a Medical Device (“SaMD”) – that manufacturers of clinical TEC products must factor into product design, testing and procurement plans.
Data protection requirements for HealthTech
Data protection and privacy remain at centre stage. In June 2025 the Information Commissioner’s Office (“ICO”) published refreshed guidance aimed squarely at manufacturers of smart products, warning that ubiquitous in-home sensors and companion devices can collect “excessive” personal information and must be designed to respect privacy by default.
The ICO’s push – coupled with the UK’s Data (Use and Access) Act coming into force – means TEC suppliers collecting and using health or behavioural data face heightened expectations on lawful basis, transparency, data minimisation and retention policies. Commissioners and care providers should expect closer ICO scrutiny where smart products are used in people’s homes.
CQC guidance on consent and surveillance
Care regulators are also clarifying how TEC fits into existing inspection and safety regimes. The Care Quality Commission has updated its assessment materials and guidance for adult social care providers on a range of areas, including patient consent, surveillance and access to digital records – emphasising that using TEC is not a substitute for lawful, person-centred practice.
Recent CQC materials make explicit that providers must obtain consent for technologies that affect a person’s privacy or dignity and must manage data and surveillance risks as part of regulatory compliance. That matters because local authorities and care providers deploying TEC now need to evidence not only clinical safety but also human-rights-aware best practice.
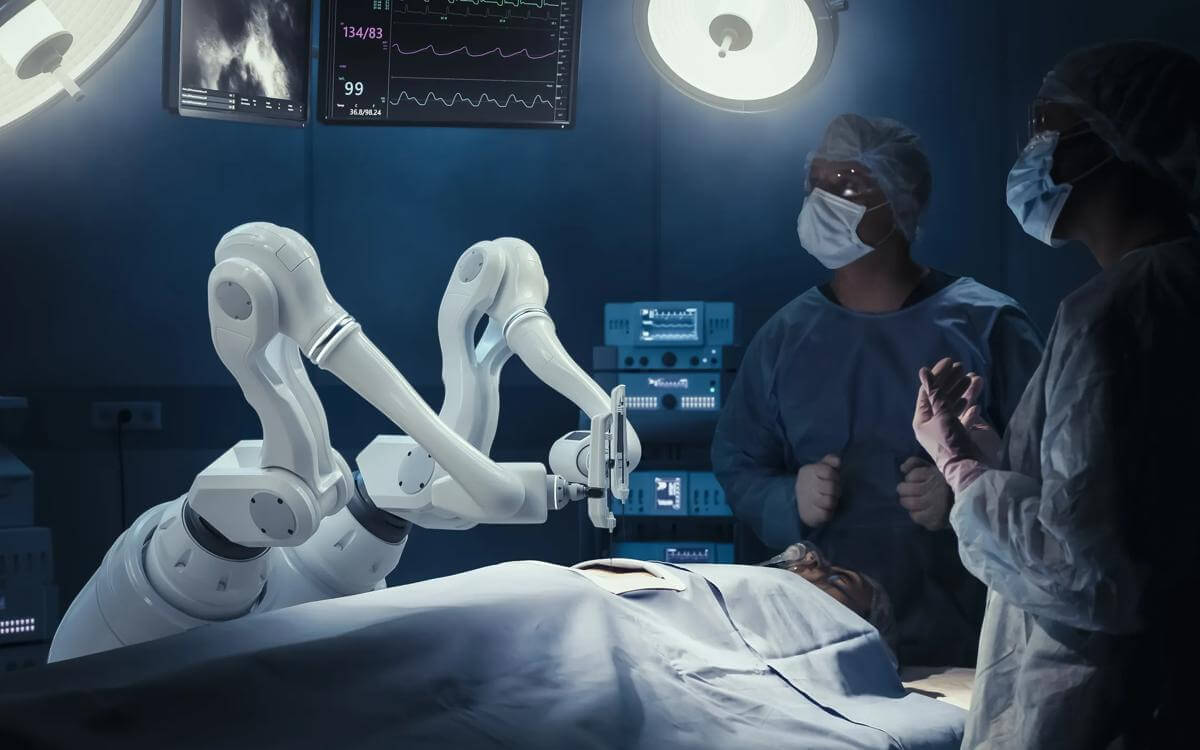
NHS England's pathway integration for technology-enabled care
Practically, NHS England has been trying to turn policy into pathways. Its ‘Technology Enabled Care’ referral guidance seeks to put TEC into urgent community response and other front-line services, helping to streamline responses and cut down the number of ambulance call outs and hospital visits.
This reflects a broader push to embed TEC in care pathways – but it also raises procurement and interoperability requirements for vendors that must integrate with digital social care records or NHS systems, where appropriate.
Three trends for TEC developers and adopters to understand
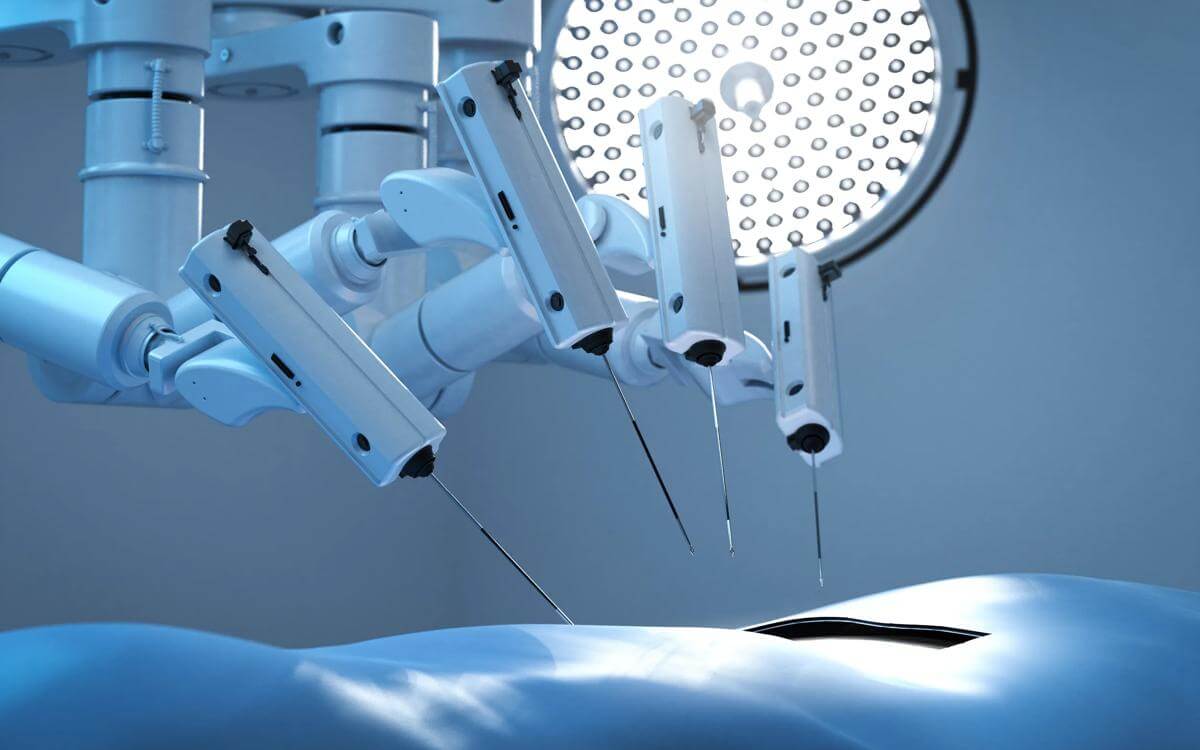
1. Cybersecurity becomes non-negotiable
MHRA and NHS procurement teams are adding cybersecurity expectations – secure update mechanisms, vulnerability management and evidence of threat modelling – to supplier checklists. The regulatory roadmap explicitly treats cybersecurity as an essential patient safety issue, as devices move from being standalone to fully connected into the digital world.
If suppliers must report serious incidents stemming from any kind of cybersecurity vulnerability to the MHRA within 15 days, they are required to track device performance and maintain records of the same to prevent regulatory censure or worse.
2. AI and adaptive software raise new validation needs
Regulators are aligning with international frameworks (for example, the International Medical Device Regulators Forum (“IMDRF”) and MHRA change programmes) that expect demonstrable clinical safety, traceability and monitoring for AI-driven features – particularly where algorithms adapt over time.
Suppliers will need stronger clinical evidence, logging and post-market monitoring that will require them to stay abreast of standardisation trends, particularly when it comes to agreeing what degree of functionality ‘change’ in machine learning tools requires such tools to be reclassified and/or recertified.
3. Privacy-first product design for the home
The ICO’s recent guidance to smart-product makers underscores design choices: minimise raw audio/video capture, process data locally where possible, offer clear on/off controls and simplify consent. These are practical, testable requirements that will influence app permissions, firmware design and product marketing.
What this means for stakeholders
- Suppliers must accelerate compliance roadmaps: build cyber and clinical safety into development lifecycles; prepare technical documentation aligned to MHRA expectations; and bake privacy-by-default into consumer devices.
- Providers and commissioners need procurement clauses covering post-market surveillance, data protection impact assessments, and incident reporting – and should demand vendor evidence on security testing, interoperability and user controls; and
- Users and carers should expect clearer information about how data will be used, applicable retention periods and the right to opt out of non-essential data collection.
The regulatory landscape is still settling. The MHRA’s roadmap is a 'living' timetable with phased deliveries and ICO guidance is prompting updates to other regulatory materials; the net result is a period where legal and technical norms will crystallise rapidly.
For a sector whose promise is to keep people safe and independent at home, that’s a healthy tension: better-defined rules mean greater public trust – provided the sector moves fast enough to embed them without stalling innovation.
Contact us
We have one of the UK’s largest health and life sciences practises with vast experience of the part technology plays in the practical application of day-to-day healthcare.
Please get in touch with our HealthTech team if you have any questions or need our help and advice.